The next investment priorities for telehealth, RPM and connected health
Healthcare IT News - Telehealth
NOVEMBER 15, 2021
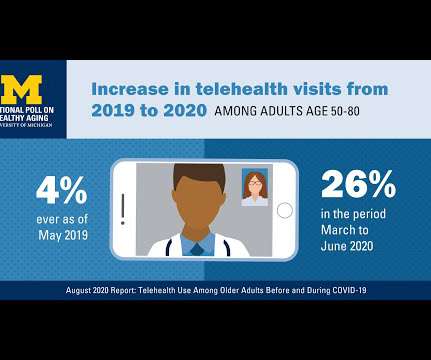
When it comes to the COVID-19 pandemic and health IT, if there's just one thing that everyone can agree on, it's that telehealth has gone mainstream. Thanks to new regulations from the government and subsequent new rules from commercial payers, telemedicine services are being reimbursed. Moore is all for telemedicine.















































Let's personalize your content