How We Spend Versus What We Get: America’s Healthcare Spending Makes for Poor Health
Health Populi
MARCH 15, 2018
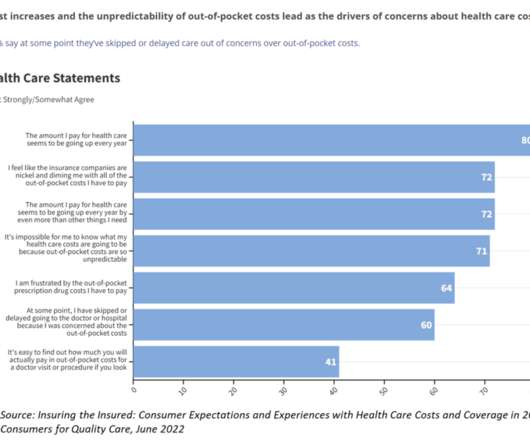
had the highest pharmaceutical spending per capita of $1,443 versus $749 for the other nations, roughly double. Access and quality of care in the U.S. varied, with that 10% of health citizens lacking coverage for basic health care.






































Let's personalize your content